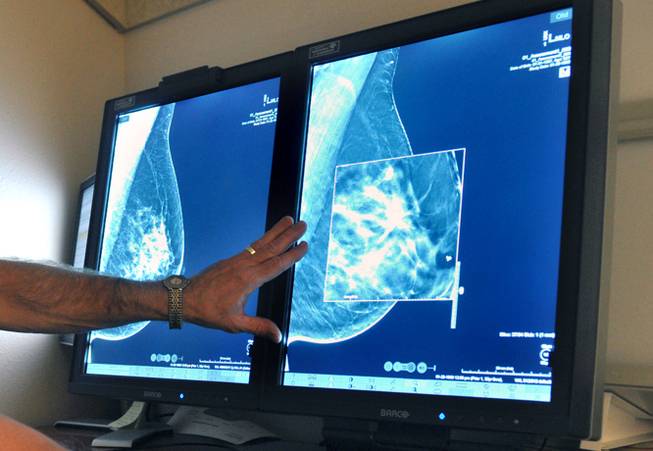
Torin Halsey/Times Record News / AP
In this Tuesday, July 31, 2012, file photo, a radiologist compares an image from earlier, 2-D technology mammogram to the new 3-D Digital Breast Tomosynthesis mammography in Wichita Falls, Texas.
Tuesday, April 9, 2024 | 2 a.m.
What can start out as just a simple lump may grow into a bigger problem down the road, and Luz Castro has seen firsthand how that can affect a person’s life.
Castro is a program manager for the Engelstad Foundation R.E.D. — Responsible Early Detection — Rose Foundation, which has provided screenings, clinical breast exams, mammograms, ultrasounds, surgical consultations and biopsies for more than 7,000 clients since its inception in the early 2000s.
At Dignity Health-St. Rose Dominican, she’s seen and supported people — especially Latina women — whose entire lives have been changed due to breast cancer, but they lived to tell the tale with early enough diagnoses.
A persistently low rate of people getting screened for breast cancer both nationally and in Southern Nevada has local organizations fighting to get breast health at the top of the public’s minds.
“We’ve tried to educate these people and these women on how it’s really important, especially in the Hispanic population, because unfortunately, we are seeing more breast cancer detections (and) diagnoses because these women don’t detect on time,” Castro said. “It’s treatable if you do something quickly.”
A mammogram is an X-ray image of the breast, which can help trained radiologists look for signs of breast cancer, according to the breast cancer awareness organization Susan G. Komen. These screenings typically take about 15 minutes, and patients can receive their results in up to two weeks, when they may need to be called back for more testing if a finding is abnormal.
Clark County falls behind the average percent of female Medicare enrollees receiving an annual mammography screening in both Nevada as well as the U.S., according to the 2024 County Health Rankings and Roadmaps published annually by the University of Wisconsin Population Health Institute.
In 2021, the most recent data used, about 32% of women enrolled in Medicare ages 65 through 74 received an annual mammography. This is below Nevada’s average of 35% of female Medicare enrollees and 43% of national ones.
Though the percentage has remained static for the past decade, the County Health Rankings and Roadmaps data shows that it has not exceeded the state or national average. Hispanic women are the least likely to receive a mammogram, with only 19% of the specific population getting tested. Native American women come in second at only 25%.
Aside from skin cancers, breast cancer is the most common cancer in American women, according to the National Breast Cancer Foundation. In 2024, an estimated 310,720 women and 2,800 men in the U.S. will be diagnosed with invasive breast cancer. There are currently over 4 million breast cancer survivors in the U.S., but an estimated 42,250 women in the U.S. will die from breast cancer this year alone.
Over half of breast cancer cases are diagnosed at a localized stage, when the cancer has yet to spread outside of the breast, making it easier to treat. The National Breast Cancer Foundation says there’s a 99% 5-year relative survival rate for cancer diagnosed at the localized stage. Early detection efforts, increased awareness and improving treatment options have helped curb the overall death rate for breast cancer.
But getting people in general to get mammogram screenings historically has been a challenge, according to local experts.
“We’re still coming back from COVID, and we’re still wanting to get people (aware) it’s important to be screened, but some people are still shy about doing that and a little bit hesitant,” said Jill Eaton, executive director of the Inland Empire, Arizona and Nevada branches of Susan G. Komen. “But we’re hoping that those numbers will continue to change.”
Castro explained that many people, especially in Hispanic culture, associate mammograms with certain negative stigma or they might simply not know they should get one.
There’s also the cost of an exam, which many low-income or undocumented people may not be able to afford if they don’t have health insurance. Plus, language barriers may prevent some non-English speakers from even seeing a primary care specialist who can refer them for a mammogram, Castro said.
The cost of a mammogram can vary depending on details like a person’s insurance coverage or location, but out-of-pocket payments could be upwards of $234 on average, according to a 2019 study conducted by The Martec Group on behalf of Susan G. Komen.
With the passage of Senate Bill 330 during the 2023 Nevada Legislature, commercial health insurers must cover annual mammograms as well as supplemental and diagnostic imaging exams at no cost to patients. Patients over 40 years old covered under Medicare and Medicaid receive yearly mammograms at no charge as well as imaging tests by methods such as MRI or ultrasound.
Additionally, Nevada Health Centers in 2000 established the Mammovan, a bright-pink semi-truck that serves as a mobile mammography unit for both insured and uninsured women age 40. Nevada Health Centers partners with companies such as CVS Health, the Breast Cancer Assistance Fund, the American Cancer Society and Susan G. Komen to bring mammogram testing to more local communities.
There’s also the work that Castro does through the R.E.D. Rose program, which helps underinsured and uninsured women access breast screening services as well as provide support for those diagnosed with breast cancer that need surgery. Funding from the R.E.D. Rose’s financial assistance program can also go toward helping pay for food, utilities, rent and chemotherapy or radiation treatment — which can cost thousands of dollars per session and disrupt the daily life of a patient, Castro said.
Castro and Eaton both stressed that mammograms were not the only way a person could check their breast health, though. The two encourage all those eligible to get mammogram screenings once a year, but they also want people to self-examine their breasts for lumps, nonitchy rashes or other abnormal signs at least once a month.
“We have to tell the community it’s not only about the family history (of breast cancer); it’s about you maintaining health and doing your regular checkups,” Castro said.
