
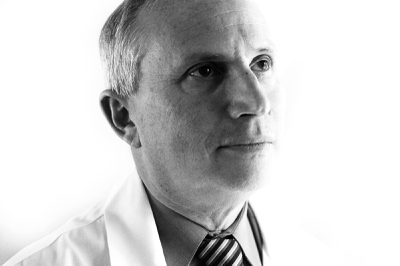
Dr. Tim McDonald, a pioneer in the patient safety movement, is co-executive director of the Institute for Patient Safety Excellence at the University of Illinois Medical Center in Chicago. “Somebody has to step up and say ‘We’re going to do this,’” he says. “It’s the smart thing to do and also happens to be the right thing to do.”
Sunday, Dec. 26, 2010 | 2 a.m.
Do No Harm: Hospital Care in Las Vegas, Part 5
- Sun investigation reveals flaws in hospital care; solutions offered
- How to put patients first
- Local hospitals’ willingness to change culture would be a step toward better care, transparency
- ‘You can’t kill my mother and get away with it’
- We must adopt a culture of sincere care
- How to file a complaint
Share your stories
Do No Harm: Brian Greenspun
Sun Publisher and Editor Brian Greenspun talks about the findings of the newspaper's series on hospital care. To address the problems raised by the series will require a change in attitude from executive suites down, including more openness with patients and a commitment to do no harm.
Dr. Tim McDonald is standing by the operating room nurses’ station, explaining how a medical error sent a patient into cardiac arrest.
He’s holding two similar medicine vials, each about the size of a thimble, with black print on white-and-lavender labels.
The medicine from the first vial can be injected as is. But the other is a concentrate. It can be deadly if not diluted. And the two bottles can be easily confused.
Five years ago, the patient, who was undergoing thoracic surgery, was accidentally injected with the concentrate. It was nearly lethal. The legal fallout could have been ugly.
But the manner in which that error was handled by the University of Illinois Medical Center in Chicago demonstrates how hospitals in Las Vegas and across the country can improve patient care.
• The hospital launched an investigation — and the patient was kept informed of its progress.
• The hospital admitted the error and apologized to the patient.
• It picked up the tab for the entire hospital stay, including the costs of the surgery during which the mistake occurred and the complications related to the overdose.
The hospital went one step further. It changed protocol so that the concentrated drug is kept in a plastic bag with the solution needed for dilution. It told accrediting agencies and other hospitals about the lesson it learned.
The patient did not sue. And the hospital has not repeated the mistake.
Such a response might be expected from a restaurant that had mixed up a food order, but it is a rare reaction for a hospital that harmed a patient. Most doctors and hospitals operate under the mentality that “it’s a mistake to admit a mistake,” because it could result in a malpractice lawsuit.
A Sun investigation — including a review of 2.9 million patient billing records filed with the state — has found Las Vegas hospitals repeatedly fail to acknowledge unsafe conditions or their mistakes, and when they harm patients they often fail to admit it or apologize. Not being forthright about safety jeopardizes patients because doctors and hospitals are not identifying and correcting mistakes or unsafe conditions that could lead to harm.
The Chicago medical center thinks patients deserve better. McDonald, an anesthesiologist, is a pioneer in the nascent patient safety movement. Co-executive director of the Institute for Patient Safety Excellence at the University of Illinois in Chicago, he grows animated when discussing the topic, pounding the table to punctuate key points.
“We have to get back to the point of restoring (patients’) trust in the system,” McDonald said. “They trust us when we start caring for them, and it’s ours to lose. If we hurt them and don’t communicate, and hide from that, we have no longer maintained or validated their trust.”
The malpractice myth
Conventional wisdom in the hospital industry holds that admitting mistakes increases malpractice lawsuits.
Counterintuitively, officials at the Chicago medical center began admitting mistakes to decrease malpractice lawsuits.
Unlike Nevada, there are no caps on medical malpractice payments in Illinois, and malpractice payouts are particularly high in Chicago. At its peak, the Chicago medical center, which is self-insured, was spending $43 million a year on malpractice-related expenses.
Research shows malpractice cases are reduced when doctors and hospitals are honest and apologetic about mistakes. In 2004 the facility’s leadership decided to be honest internally and with patients about unsafe conditions, close calls and instances of patient harm. Skeptics thought it would usher in a malpractice Apocalypse.
The pro-patient philosophy encompasses seven guidelines or pillars:
• Incident reporting: The vast majority of reports are cases of unsafe conditions or close calls where patients could have been harmed.
• Investigation: Every report is investigated within 72 hours, and no findings are withheld from the patient and family.
• Disclosure and communication: The hospital maintains open communication with the patient and family until the issue is resolved.
• Apology and remediation: When the hospital does not meet the standard of care, resulting in harm to a patient, it apologizes and offers some sort of solution to the problem. In the most extreme cases, compensation is extended.
• System improvements: The staff takes steps to prevent the recurrence of the problem.
• Data tracking and analysis: The hospital collects and analyzes patient safety incidents to improve quality and prevent harm.
• Education and training: Doctors, nurses, administrators and support staff take annual competency exams and attend monthly patient safety meetings and other training.
The “seven pillars” program is “extremely comprehensive and broad,” McDonald said. It’s infused in the hospital’s culture from the executive suite to the front lines.
Program leaders have a mantra to describe their approach to physician compliance with the program: “Educate the young and regulate the old.” Patient safety is a focal point of the curriculum from Day One at the University of Illinois at Chicago College of Medicine. And older doctors — not accustomed to admitting mistakes and sitting atop the medical hierarchy — may need regulation to be accountable.
From 2006 to 2008, the Chicago hospital had about 2,400 patient safety incident reports, 766 cases where patients were harmed and 20 full disclosures of inappropriate or unreasonable care that caused harm, where compensation was offered.
Hospital lawyers and administrators are pleased with the results. Malpractice claims have dropped 30 percent and overall malpractice costs have been cut by $3 million a year to about $40 million. Danny Chun, spokesman for the Illinois Hospital Association, said he has not heard of another hospital in the state that has reduced malpractice costs.
McDonald credits the openness and humility for eliminating frivolous lawsuits. The investigation into each event is open, so patients would not need to sue just to get information, he said. And they have the satisfaction of becoming part of the solution to the problems that caused the harm.
“I’ve always felt badly that our motivation had to be financial,” said Dr. William Chamberlin, chief medical director of the facility. “But now I would argue that full disclosure will help improve the safety.”
Confronting the truth
In 2008, a young mother was under conscious sedation during a procedure at the Chicago medical center when she went into respiratory failure and cardiac arrest. She died.
In investigating the case, staff found the facility had not monitored her carbon dioxide levels because it was not required, which made it difficult to notice when she stopped breathing. The nurses’ response was also subpar.
The tragedy brought safety improvements to such procedures:
• Carbon dioxide levels are monitored.
• An anesthesiologist fully sedates the patient.
• Nurses have been retrained in how to respond to cardiac arrest.
In addition, the woman’s father sits on the hospital’s patient safety committee, helping hold the facility accountable for improving care. The family did not want to be interviewed.
Dr. David Schwartz, head of the hospital’s anesthesiology department, was not present during this incident, but shared with the family the findings of the investigation and apologized on behalf of the hospital.
“It’s gut-wrenching and stays with you your whole life,” he said recently. “We’ve all made errors. In our field, you make an error and someone can die. It’s devastating. You feel worthless. You play the scenario over and over again in your mind.”
Patient safety also means encouraging staff to challenge superiors.
Surgeons were about to sew up a patient after a late-night emergency liver transplant this year when nurses Tessie Trocio and Noemi Tueres noticed during their routine count that a thin, flat sponge — about the size of a sheet of paper — was missing. Protocol called for an abdominal X-ray to rule out any retained objects, but the image was inconclusive. The nurses demanded another X-ray, which showed nothing in the abdomen.
Nurses are often hesitant to challenge doctors, particularly in the operating room. And in this case, the nurses were trained in the Philippines, where the cultural tendency is to not challenge authority.
The operation had taken more than seven hours. The surgeons were waiting. But the nurses — on their hands and knees digging through the trash to find the missing sponge — demanded a third X-ray, and that it be read by a radiologist.
The sponge was identified, balled up behind the liver. It was safely removed.
“That was a medical save,” said Kathy Pinschke Winn, the hospital’s professional development coordinator. “That patient would not have survived.”
The case was celebrated throughout the hospital, in a newsletter and at a luncheon to honor the nurses, Winn said.
Reports of harm, close calls or unsafe conditions can be anonymous and may be submitted in handwritten notes, over the phone, online or in person. Doctors are trained on the reporting process. And if the hospital learns of a problem through a lawsuit — when it may be too late to resolve easily — the clinical departments that failed to report the incident are penalized financially.
A risk manager is on duty 24 hours a day to investigate reports. The scrutiny builds confidence in the program among front-line staff, said Nikki Centomani, the hospital’s safety and risk management director. If reports are not followed up, employees will lose confidence and stop filing them, she said.
Since the program began, the number of reports has jumped more than fourfold to 7,000 a year.
Eliminating the “shame and blame” that traditionally comes with identifying problems is a key to reporting, said Dr. David Mayer, who leads the patient safety institute with McDonald.
The majority of problems are because of unsafe conditions and practices that have become endemic, he said.
“Good people are being put into systems or processes that are designed for bad things to happen,” he said.
Most of the reports do not involve patient harm, and Mayer refers to each as a “gift” — “an opportunity to protect somebody.”
From 2006 to 2008, the guidelines have triggered more than 200 patient safety improvements.
Expanding the seven pillars
The patient safety program is expanding, thanks to a $3 million federal grant to the center in June. The funding is part of a broader initiative announced by President Barack Obama in 2009 to invest in new ways to address medical malpractice. The expansion will begin with about 10 Chicago hospitals, some investor-owned, as are most of the facilities in Las Vegas.
One of them, MacNeal Hospital, is a 427-bed, for-profit facility owned by Tennessee-based Vanguard Health System, which also owns facilities in Arizona, Massachusetts and Texas.
Dr. Charles Bareis, MacNeal’s chief medical officer, said it needs to improve communication with patients. “The standard response is ‘Don’t talk to anyone about this, hunker down and see if they sue,’ ” he said. “It’s not good for patients and families and destroys the morale of your staff.”
Bareis said if the seven pillars succeed at MacNeal, there is interest in expanding it throughout the chain.
Success will be measured primarily by whether the program saves the hospital money, he said, but implementing it is right for patient safety and for employees. He said he’s less concerned with the hospital’s motive than he is with moving in the right direction.
Similar to Las Vegas hospitals, most doctors at MacNeal are not on salary at the facility, and are insured against medical malpractice by a different company than the hospital. When Bareis talks to doctors about implementing the seven pillars, they don’t disagree, he said. Instead, they support the program because so many patients have been harmed, he said.
Being transparent by conducting open investigations, admitting mistakes and apologizing is satisfying for caregivers, Bareis said. It puts them where they belong, on the same team with the patient.
Hospitals in other states are interested in adopting the seven pillars. Alfred Gilchrist, CEO of the Colorado Medical Society, said doctors and hospital administrators in his state are discussing the program, which he calls “an enlightened evolution.”
He has advocated for medical malpractice caps favored by doctors in Nevada and other states, but sees them as limited in effectiveness.
“Tort reform is a blunt instrument,” Gilchrist said. “Has it made the system safer? Has it made doctors more accountable? Has it restored people who are hurt? I don’t think so.”
McDonald said the seven pillars “could and should be done in Las Vegas.” They require courage and leadership on the part of doctors and hospital administrators to make a commitment that patient safety will become central to the delivery of medical care, he said. The biggest barrier is fear — of the unknown, of financial ruin and of loss of reputation. But those can be overcome, he said.
“Somebody has to step up and say ‘We’re going to do this,’ ” McDonald said. “It’s the smart thing to do and also happens to be the right thing to do.”






Join the Discussion:
Check this out for a full explanation of our conversion to the LiveFyre commenting system and instructions on how to sign up for an account.
Full comments policy